From Bioblast
| Healthy reference population | Body mass excess | BFE | BME cutoffs | BMI | H | M | VO2max | mitObesity drugs |
Body mass excess and mitObesity
Communicated by Gnaiger Erich (2020-02-12) last update 2020-07-06 in: Catastrophe XXX XXX-mass Carol on BME and mitObesity of X-mass Carol
Summary
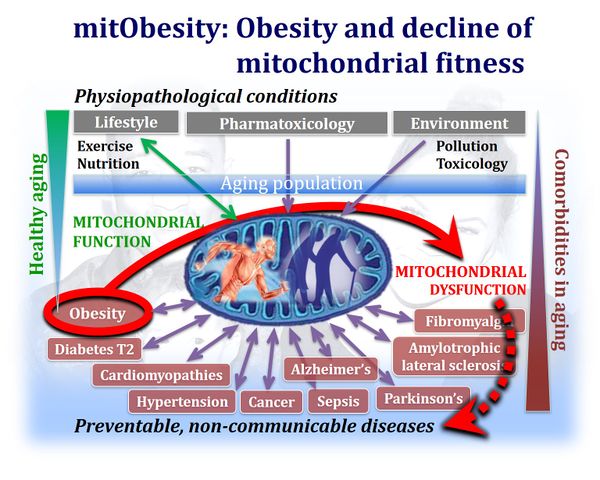
- Obesity is a world-wide epidemic with severe consequences on the health of our modern aging populations, linked to several comorbidities by mechanisms that remain largely obscure. The decline of mitochondrial fitness in overweight states is a biomarker of the systemic mitObesity syndrome, providing a mechanistic link between common obesity and associated chronic comorbidities — such as diabetes, hypertension and chronic heart failure, neurodegenerative diseases and several types of cancer. Today mitObesity is the world-wide leading cause of deaths and early aging, which can be prevented by an active lifestyle with physical exercise and caloric balance.
Events on mitObesity
- 2023 Jun 06: » Health Innovation Summit 2023 Vienna AT
BME and mitObesity news
- 2020-05-05 Obesity and COVID-19 severity
- Since the decline of mitochondrial respiratory function is strongly associated with obesity (mitObesity), health practitioners have to be made aware of the potential role played by obesity and mitochondrial dysfunction in determining COVID-19 severity. For references, see: »Viruses and mitochondrial medicine«.
- 2020-02-18 Spermidine added to mitObesity drugs
- Tyrrell DJ, Blin M, Song J, Wood S, Zhang M, Beard DA, Goldstein D (2019) Age-associated mitochondrial dysfunction accelerates atherogenesis. Circ Res 126:298–314. - »Bioblast link«
- The BMI paradigm - time for a change
- 2020-02-15 updated: BME cutoff points
- 'The robustness of the BMI-mortality relationship reflects the numerous health conditions and co-morbidities associated with an elevated BMI.' - In BMI we trust: reframing the body mass index as a measure of health » Gutin 2018 Soc Theory Health
- The double burden of malnutrition 'is the coexistence of overnutrition (overweight and obesity) alongside undernutrition (stunting and wasting), at all levels of the population—country, city, community, household, and individual." - The double burden of malnutrition. The Lancet (Published: December 16, 2019) - Open Access
- 'Despite being weakly associated with adiposity, the simple anthropometric BMI provides a useful metabolic risk marker for populations.8 The main limitation of BMI is its inconsistent association with non-communicable disease risk across populations.' » Wells 2020 Lancet
- Embracing a positive lifestyle as prescription for an extended health span » Pizzo 2020 JAMA
- Obesity and cardiovascular comorbidities
- Comorbid cardiovascular diseases and major psychiatric disorders associated with obesity. - 'People with major psychiatric disorders (MPDs) have a 10- to 20-year shorter life span than the rest of the population, and this difference is mainly due to comorbid cardiovascular diseases. .. overlapping loci are involved in several pathways including neurodevelopment, neurotransmitter signaling, and intracellular processes ..' » Bahrami 2020 JAMA Psychiatry
- Obstructive physiology linked to obesity in patients with hypertrophic cardiomyopathy » Fumagalli 2019 JAMA Cardiol
- Obesity, psychiatric and neurodegenerative disorders
- Aerobic and strength training protect from peripheral comorbidities in Alzheimer’s disease » Pena 2020 Int J Chronic Dis
- From obesitiy in mothers to psychiatric disorders in children with median age of ontset from 1 to 7 years - are mitochonrial genes involved? - '.. pregestational type 2 diabetes in severely obese mothers was associated with several psychiatric disorders in their offspring. .. Diabetes in normal-weight mothers was not associated with psychopathologic disorders in the offspring.' » Kong 2020 JAMA Netw Open
- BMI and depression » Khan 2020 Cureus
- BMI surveillance over time provides a strong predictor of BMI over a period of 25 years - 'close clinical surveillance and fitness may have prime roles in limiting the adverse consequences of elevated BMI on health.' » Murthy 2020 JAMA Cardiol
- Solving the obesity epidemic: is artificial intelligence the answer? - https://www.openaccessgovernment.org/ai-solving-the-obesity-epidemic/81671/
| Link | BME and mitObesity news: Literature - last update 2020-02-18 |
|---|---|
| Bahrami 2020 JAMA Psychiatry | Bahrami S, Steen NE, Shadrin A, O'Connell K, Frei O, Bettella F, Wirgenes KV, Krull F, Fan CC, Dale AM, Smeland OB, Djurovic S, Andreassen OA (2020) Shared genetic loci between body mass index and major psychiatric disorders: a genome-wide association study. JAMA Psychiatry 2020 Jan 8. doi: 10.1001/jamapsychiatry.2019.4188. |
| Bhatraju 2020 N Engl J Med | Bhatraju Pavan K, Ghassemieh Bijan J, Nichols Michelle, Kim Richard, Jerome Keith R, Nalla Arun K, Greninger Alexander L, Pipavath Sudhakar, Wurfel Mark M, Evans Laura, Kritek Patricia A, West T Eoin, Luks Andrew, Gerbino Anthony, Dale Chris R, Goldman Jason D, O’Mahony Shane, Mikacenic Carmen (2020) Covid-19 in critically ill patients in the Seattle region - case series. N Engl J Med 2020;NEJMoa2004500 [published online ahead of print, 2020 Mar 30]. |
| Chambers 2020 J Appl Physiol (1985) | Chambers TL, Burnett TR, Raue U, Lee GA, Finch WH, Graham BM, Trappe TA, Trappe S (2020) Skeletal muscle size, function, and adiposity with lifelong aerobic exercise. J Appl Physiol (1985) 128:368–78. |
| Corlin 2020 JAMA Cardiol | Corlin Laura, Short Meghan I, Vasan Ramachandran S, Xanthakis Vanessa (2020) Association of the duration of ideal cardiovascular health through adulthood with cardiometabolic outcomes and mortality in the Framingham offspring study. JAMA Cardiol Published online March 11, 2020. |
| Fumagalli 2019 JAMA Cardiol | Fumagalli C, Maurizi N, Day SM, Ashley EA, Michels M, Colan SD, Jacoby D, Marchionni N, Vincent-Tompkins J, Ho CY, Olivotto I, SHARE Investigators (2019) Association of obesity with adverse long-term outcomes in hypertrophic cardiomyopathy. JAMA Cardiol 2019 Nov 6:1-8. doi: 10.1001/jamacardio.2019.4268. |
| Gutin 2018 Soc Theory Health | Gutin I (2018) In BMI we trust: reframing the body mass index as a measure of health. Soc Theory Health 16:256–71. |
| Khan 2020 Cureus | Khan QU, Zaffar S, Rehan AM, Rashid RR, Ashraf H, Hafeez F (2020) Relationship of major depression with body mass index and salivary cortisol. Cureus 12:e6577. |
| Kong 2020 JAMA Netw Open | Kong L, Nilsson IAK, Brismar K, Gissler M, Lavebratt C (2020) Associations of different types of maternal diabetes and body mass index with offspring psychiatric disorders. JAMA Netw Open 2020 Feb 5;3(2):e1920787. |
| Korre 2016 Am J Cardiol | Korre M, Porto LG, Farioli A, Yang J, Christiani DC, Christophi CA, Lombardi DA, Kovacs RJ, Mastouri R, Abbasi S, Steigner M, Moffatt S, Smith D, Kales SN (2016) Effect of body mass index on left ventricular mass in career male firefighters. Am J Cardiol 118:1769-1773. |
| Madeo 2018 Science | Madeo F, Eisenberg T, Pietrocola F, Kroemer G (2018) Spermidine in health and disease. Science 359:eaan2788. |
| Murthy 2020 JAMA Cardiol | Murthy VL, Xia R, Baldridge AS, Carnethon MR, Sidney S, Bouchard C, Sarzynski MA, Lima JAC, Lewis GD, Shah SJ, Fornage M, Shah RV (2020) Polygenic risk, fitness, and obesity in the Coronary Artery Risk Development In Young Adults (CARDIA) study. JAMA Cardiol 5:40-8. doi: 10.1001/jamacardio.2019.5220 |
| Pena 2020 Int J Chronic Dis | Pena GS, Paez HG, Johnson TK, Halle JL, Carzoli JP, Visavadiya NP, Zourdos MC, Whitehurst MA, Khamoui AV (2020) Hippocampal growth factor and myokine cathepsin B expression following aerobic and resistance training in 3xTg-AD mice. Int J Chronic Dis 2020:Article ID 5919501. |
| Petrilli 2020 medRxiv | Petrilli Christopher M, Jones Simon A, Yang Jie, Rajagopalan Harish, O'Donnell Luke F, Chernyak Yelena, Tobin Katie, Cerfolio Robert J, Francois Fritz, Horwitz Leora I (2020) Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City. medRxiv doi: https://doi.org/10.1101/2020.04.08.20057794 . |
| Pizzo 2020 JAMA | Pizzo PA (2020) A prescription for longevity in the 21st century: renewing purpose, building and sustaining social engagement, and embracing a positive lifestyle. JAMA 2020 Jan 9. doi: 10.1001/jama.2019.21087. |
| Popkin 2020 Lancet | Popkin BM, Corvalan C, Grummer-Strawn LM (2020) Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 395:65-74. |
| Qingxian 2020 Lancet | Qingxian Cai, Chen Fengjuan, Fang Luo, Xiaohui Liu, Tao Wang, Qikai Wu, Qing He, Zhaoqin Wang, Yingxia Liu, Jun Chen, Lei Liu, Lin Xu (2020) Obesity and COVID-19 severity in a designated hospital in Shenzhen, China. Lancet Preprint at SSRN https://doi.org/10.2139/ssrn.3556658. |
| Stefan 2020 Nat Rev Endocrinol | Stefan N, Birkenfeld AL, Schulze MB, Ludwig DS (2020) Obesity and impaired metabolic health in patients with COVID-19. Nat Rev Endocrinol 2020:1‐2 [published online ahead of print, 2020 Apr 23]. |
| Tyrrell 2019 Circ Res | Tyrrell DJ, Blin M, Song J, Wood S, Zhang M, Beard DA, Goldstein D (2019) Age-associated mitochondrial dysfunction accelerates atherogenesis. Circ Res 126:298–314. |
| Wells 2020 Lancet | Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, Demaio A (2020) The double burden of malnutrition: aetiological pathways and consequences for health. Lancet 395:75-88. |
| Yang 2019 JAMA Netw Open | Yang J, Christophi CA, Farioli A, Baur DM, Moffatt S, Zollinger TW, Kales SN (2019) Association between push-up exercise capacity and future cardiovascular events among active adult men. JAMA Netw Open 2019;2:e188341. |
mitObesity and comorbidities: body mass excess and decline of mitochondrial fitness
Work in progress by Gnaiger E 2020-02-14 linked to a preprint in preparation on body mass excess, BME and mitObesity.
Executive summary
- The decline of muscular mitochondrial fitness in overweight states is a biomarker of the systemic mitObesity syndrome: Compromised mitochondrial fitness across metabolically active organs provides the mechanistic link between common obesity and associated chronic comorbidities — such as diabetes, hypertension and chronic hear failure, neurodegenerative diseases and several types of cancer — bound to redox imbalance, inflammation, oxidative stress and derangement of glucose/fatty acid homeostasis. Today mitObesity is the world-wide leading cause of deaths and early aging, which can be prevented by an active lifestyle and improvement of the quality of life by exercise and caloric balance with healthy food.
- The WHO defines obesity by convention as a body mass index, BMI, equal or above 30 kg·m-2. The BMI has been critizised, however, as an indicator of obesity due to its poor correlation with body fat expressed as percent body fat mass per total body mass, BF%. Another fundamental limitation of the BMI as a general index of obesity is the fact that BMI cutoff points — evaluated primarily in adult male Caucasian populations — have to be adjusted for Asian populations, where distinct BMI cutoff points are discussed for women and men. Should sex differences in BMI cutoffs be considered in all populations irrespective of ethnic background? BMI cutoffs are dramatically different in children and adolescents. These limitations or complications of the BMI are addressed collectively by the concept of body mass excess, BME, with respect to the healthy reference population: (1) The BME correlates linearly and tightly with body fat excess equally in women and men. (2) BME cutoff points for overweight and obese are identical in a wide range of evolutionary (ethnic) backgrounds including European and American white Caucasians, American blacks, and Asian populations, strictly by considering the body mass/height allometry in the healthy reference population. (3) BME cutoff points apply equally to adult women and men, adolescents and children, considering four allometric phases in human growth.
- 20 % and 40 % in excess of the reference body mass at a given height are the BME cutoff points for overweight and obese, BME = 0.2 and 0.4, respectively. Compared to the BMI, the BME cutoff points can be more easily communicated and understood by non-experts. Only specialists, however, are familiar with the meaning of gender-, age- and population-adjusted values of BMI cutoff points (Footnote a). Nevertheless, precision-BMI cutoff points are derived for harmonization of BMI and BME concepts.
- In contrast to obesity, the devastating effects on health of starvation and undernutrition (negative BME) are bound to entirely different systemic and molecular mechanisms. In statistical studies, therefore, it is inappropriate to calculate the average or median BME of the total population, but the underweight (BME < -0.1) and overweight (BME > 0.2) subpopulations have to be separated from the reference group (BME = -0.1 to 0.2) for comparison and evaluation of health risks.
- The decline of mitochondrial fitness in skeletal muscle is tightly associated with the body mass excess, BME, in healthy populations in the succession from the reference BME to overweight and obese BME states. The decline of mitochondrial fitness is non-linearly related to the progressive loss of cardiorespiratory fitness with increasing BME, measured as maximum ergometric aerobic capacity per total body mass, VO2max/M. The systemic decline of mitochondrial respiratory fitness is a hallmark of mitObesity.
- Several drugs and nutraceuticals with more or less reproducible beneficial effects in the treatment of diverse preventable degenerative diseases implicated in comorbidities have common mechanisms of action targeting mitochondria. These medications and neutraceuticals — such as metformin, melatonin, flavonoids, curcumin, resveratrol, spermidine, Coenzyme Q- or ubiquinol-linked drugs (MitoQ, SkQ, CoQ10), Rapamycin, Elamipretide (Bendavia) — can be classified as bioactive mitObesity compounds, providing strong evidence for the role of mitochondria-linked mechanisms of action underlying the mitObesity syndrome. Metformin has been introduced as the drug of choice for the treatment of type 2 diabetes and is particularly effective in obese patients. Today metformin and melatonin are discussed in cancer therapy, prevention of neurodegenerative diseases and cardiac ischemia-reperfusion injury, becoming prototypes of so-called anti-aging drugs. Recognition of the mitObesity syndrome may shed new light on the mysteries of anti-aging therapies, with BME and mitochondrial dysfunction implicated in vicious cause-and-effect feedback cycles.
- The resolution of preclinical studies and clinical trials, which have been based in the past on BMI matching, may have been limited by insufficient matching of BME in experimental and placebo control groups. Similarly, gender medicine in the prevailing context of obesity has been biased when using common BMI cutoffs, which ignore the allometric effect of differences in height on precision-BMI cutoffs revealed by the BME concept. Importantly, the personal history of prevalence of body mass excess constitutes an important element in risk assessment.
- Caloric balance in a physically active lifestyle constitutes the evolutionary background of indigenous peoples, who by adhering to traditional lifestyles in fact prevent preventable degenerative diseases. In modern societies with progressive life time expansion, a physically active lifestyle and caloric balance — by avoiding excessive consumption of low-quality food and drinks — present the most successful and promising approaches to address the pandemic obesity crisis. This requires implementation of sociopolitical strategies and governance on economic best practice: to combat the threats of mitObesity on the health care systems of high-income and low-income countries alike, our modern world's deadly obesogenic drivers must be kept in check, parallel to and synergistic with a focus on climate change and environmental protection.
Footnote
- (a) "The cutoffs for undernutrition are defined as follows: a weight-for-height Z score of less than –2 for wasting; a height-for-age Z score of less than –2 for children aged 0–4 years for stunting; and a body-mass index (BMI) of less than 18∙5 kg/m² for thinness in adult women. For overweight, the cutoffs are a BMI Z score of greater than 2 in children younger than 18 years, and a BMI of greater than 25 kg/m² in more than 20 %, 30 %, or 40 % of the adult (older than 18 years) population35 (figure 1; appendix pp 6–11). We use a combination of overweight and obesity because extensive epidemiological research associates BMI of 25 kg/m² or higher (or possibly an even lower threshold) with the risks of noncommunicable diseases across LMICs.36–42" - Popkin 2020 Lancet
MitoPedia: BME and mitObesity
» Body mass excess and mitObesity | BME and mitObesity news | Summary |
| Term | Abbreviation | Description |
|---|---|---|
| BME cutoff points | BME cutoff | Obesity is defined as a disease associated with an excess of body fat with respect to a healthy reference condition. Cutoff points for body mass excess, BME cutoff points, define the critical values for underweight (-0.1 and -0.2), overweight (0.2), and various degrees of obesity (0.4, 0.6, 0.8, and above). BME cutoffs are calibrated by crossover-points of BME with established BMI cutoffs. |
| Body fat excess | BFE | In the healthy reference population (HRP), there is zero body fat excess, BFE, and the fraction of excess body fat in the HRP is expressed - by definition - relative to the reference body mass, M°, at any given height. Importantly, body fat excess, BFE, and body mass excess, BME, are linearly related, which is not the case for the body mass index, BMI. |
| Body mass | m [kg]; M [kg·x-1] | The body mass M is the mass (kilogram [kg]) of an individual (object) [x] and is expressed in units [kg/x]. Whereas the body weight changes as a function of gravitational force (you are weightless at zero gravity; your floating weight in water is different from your weight in air), your mass is independent of gravitational force, and it is the same in air and water. |
| Body mass excess | BME | The body mass excess, BME, is an index of obesity and as such BME is a lifestyle metric. The BME is a measure of the extent to which your actual body mass, M [kg/x], deviates from M° [kg/x], which is the reference body mass [kg] per individual [x] without excess body fat in the healthy reference population, HRP. A balanced BME is BME° = 0.0 with a band width of -0.1 towards underweight and +0.2 towards overweight. The BME is linearly related to the body fat excess. |
| Body mass index | BMI | The body mass index, BMI, is the ratio of body mass to height squared (BMI=M·H-2), recommended by the WHO as a general indicator of underweight (BMI<18.5 kg·m-2), overweight (BMI>25 kg·m-2) and obesity (BMI>30 kg·m-2). Keys et al (1972; see 2014) emphasized that 'the prime criterion must be the relative independence of the index from height'. It is exactly the dependence of the BMI on height - from children to adults, women to men, Caucasians to Asians -, which requires adjustments of BMI-cutoff points. This deficiency is resolved by the body mass excess relative to the healthy reference population. |
| Comorbidity | Comorbidities are common in obesogenic lifestyle-induced early aging. These are preventable, non-communicable diseases with strong associations to obesity. In many studies, cause and effect in the sequence of onset of comorbidities remain elusive. Chronic degenerative diseases are commonly obesity-induced. The search for the link between obesity and the etiology of diverse preventable diseases lead to the hypothesis, that mitochondrial dysfunction is the common mechanism, summarized in the term 'mitObesity'. | |
| Healthy reference population | HRP | A healthy reference population, HRP, establishes the baseline for the relation between body mass and height in healthy people of zero underweight or overweight, providing a reference for evaluation of deviations towards underweight or overweight and obesity. The WHO Child Growth Standards (WHO-CGS) on height and body mass refer to healthy girls and boys from Brazil, Ghana, India, Norway, Oman and the USA. The Committee on Biological Handbooks compiled data on height and body mass of healthy males from infancy to old age (USA), published before emergence of the fast-food and soft-drink epidemic. Four allometric phases are distinguished with distinct allometric exponents. At heights above 1.26 m/x the allometric exponent is 2.9, equal in women and men, and significantly different from the exponent of 2.0 implicated in the body mass index, BMI [kg/m2]. |
| Height of humans | h [m]; H [m·x-1] | The height of humans, h, is given in SI units in meters [m]. Humans are countable objects, and the symbol and unit of the number of objects is N [x]. The average height of N objects is, H = h/N [m/x], where h is the heights of all N objects measured on top of each other. Therefore, the height per human has the unit [m·x-1] (compare body mass [kg·x-1]). Without further identifyer, H is considered as the standing height of a human, measured without shoes, hair ornaments and heavy outer garments. |
| Length | l [m] | Length l is an SI base quantity with SI base unit meter m. Quantities derived from length are area A [m2] and volume V [m3]. Length is an extensive quantity, increasing additively with the number of objects. The term 'height' h is used for length in cases of vertical position (see height of humans). Length of height per object, LUX [m·x-1] is length per unit-entity UX, in contrast to lentgth of a system, which may contain one or many entities, such as the length of a pipeline assembled from a number NX of individual pipes. Length is a quantity linked to direct sensory, practical experience, as reflected in terms related to length: long/short (height: tall/small). Terms such as 'long/short distance' are then used by analogy in the context of the more abstract quantity time (long/short duration). |
| MitObesity drugs | Bioactive mitObesity compounds are drugs and nutraceuticals with more or less reproducible beneficial effects in the treatment of diverse preventable degenerative diseases implicated in comorbidities linked to obesity, characterized by common mechanisms of action targeting mitochondria. | |
| Obesity | Obesity is a disease resulting from excessive accumulation of body fat. In common obesity (non-syndromic obesity) excessive body fat is due to an obesogenic lifestyle with lack of physical exercise ('couch') and caloric surplus of food consumption ('potato'), causing several comorbidities which are characterized as preventable non-communicable diseases. Persistent body fat excess associated with deficits of physical activity induces a weight-lifting effect on increasing muscle mass with decreasing mitochondrial capacity. Body fat excess, therefore, correlates with body mass excess up to a critical stage of obesogenic lifestyle-induced sarcopenia, when loss of muscle mass results in further deterioration of physical performance particularly at older age. | |
| VO2max | VO2max; VO2max/M | Maximum oxygen consumption, VO2max, is and index of cardiorespiratory fitness, measured by spiroergometry on human and animal organisms capable of controlled physical exercise performance on a treadmill or cycle ergometer. VO2max is the maximum respiration of an organism, expressed as the volume of O2 at STPD consumed per unit of time per individual object [mL.min-1.x-1]. If normalized per body mass of the individual object, M [kg.x-1], mass specific maximum oxygen consumption, VO2max/M, is expressed in units [mL.min-1.kg-1]. |
Labels: MiParea: Respiration, mt-Biogenesis;mt-density, Gender, Exercise physiology;nutrition;life style, mt-Medicine Pathology: Obesity
Organism: Human
BME
Further pages with specific details
Pages in category ""
The following 13 pages are in this category, out of 13 total.